Playing is Learning
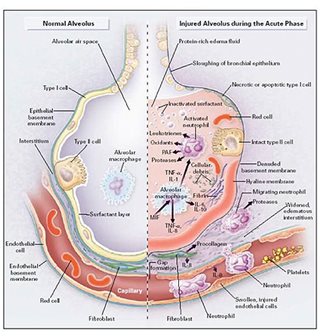
The Pathogenesis of acute lung injury
October 11th, 2016
| Ads | ||
|
Play the Challenge
|
||
|
A New Word is Coined A new Character is revealed A new Game is Afoot |
An Edutainment Adventure Based on Three Rounds of Investigations
|
|
|
Welcome to the World of PROFESsee™by seeCOSM™ PROFESsee™ is my title. I am the perpetual learner, in pursuit of knowledge, wisdom and truth. I derived my name from professor |
 |
|
|
Acute lung injury is akin to a land's invasion by foreign elements. These foreign elements ravage, ransack, and damage the very essence of the land. A quick example is ISIS and the destruction they leave in their wake. Even when (and I pray soonest) wiped out, the damage done will take years if not centuries to amend. Likewise with acute lung injury, there is an invasion that begets the presence of foreign elements in the lung, whose continued presence wreak havoc on the components of the lungs. If all these sound literature-esque, give me the next paragraphs to explain better. The onset of acute lung injury is caused by trauma or infection. Either of the two can result in microvascular endothelial injury. This injury makes the capillary more permeable. Increased permeability puts the lung at risk, and indeed, there is an influx of protein-rich plasma into the interstitium. With only time as a constraint, soon, the protein-rich plasma finds its way past the epithelial barrier – the boundary between the interstitium and the Alveolar air space. The cells of the epithelial barrier had been held together by the bond of the junctions between the type I and type II alveolar cells. The increased permeability damages and puts a strain on the epithelial barrier regulating functions of the type I and type II cells. The damage to these cells causes a change in the fluid transport of the lung. Rather than an up-regulation of the epithelial channels (Na, Na + /K + ATPase pumps), there is a down-regulation. With this in place, the repair or the reversal of the protein-rich plasma influx into the Alveolar air space cannot be achieved internally. The breach in the epithelial membrane causes what is known as the transepithelial neutrophil migration. The neutrophils invasion into the Alveolar air space is key, in the sense that it is the neutrophils that mostly and primarily cause inflammation. There continued presence plays out in four primary ways. First, they cause the increase in the endothelial barrier permeability and causes the destruction of the epithelial basement barrier (imagine an unprotected border). They also release mediators that cause inflammations on adjacent cells. Lastly, migrating neutrophils enlarge the interstitium – their migratory path. Can you Assemble the affected lung components? Image courtesy of: https://www.uichildrens.org/childrens-content.aspx?id=234103 |
||
Latest News / Events
E-mail [email protected]
The Professee™ Newsletter Beta
http://www.seecosm.com/
http://www.seecosm.com/

